Chronic Tendon Pathology

Tendinopathy
Tendinopathy can develop when you injure or overuse a tendon. Although tendinopathy can become chronic, your symptoms will likely improve with rest and physical therapy.
What is tendinopathy?
Tendinopathy is the broad term for any tendon condition that causes pain and swelling. When your muscles tighten and relax, your tendons and bones move.
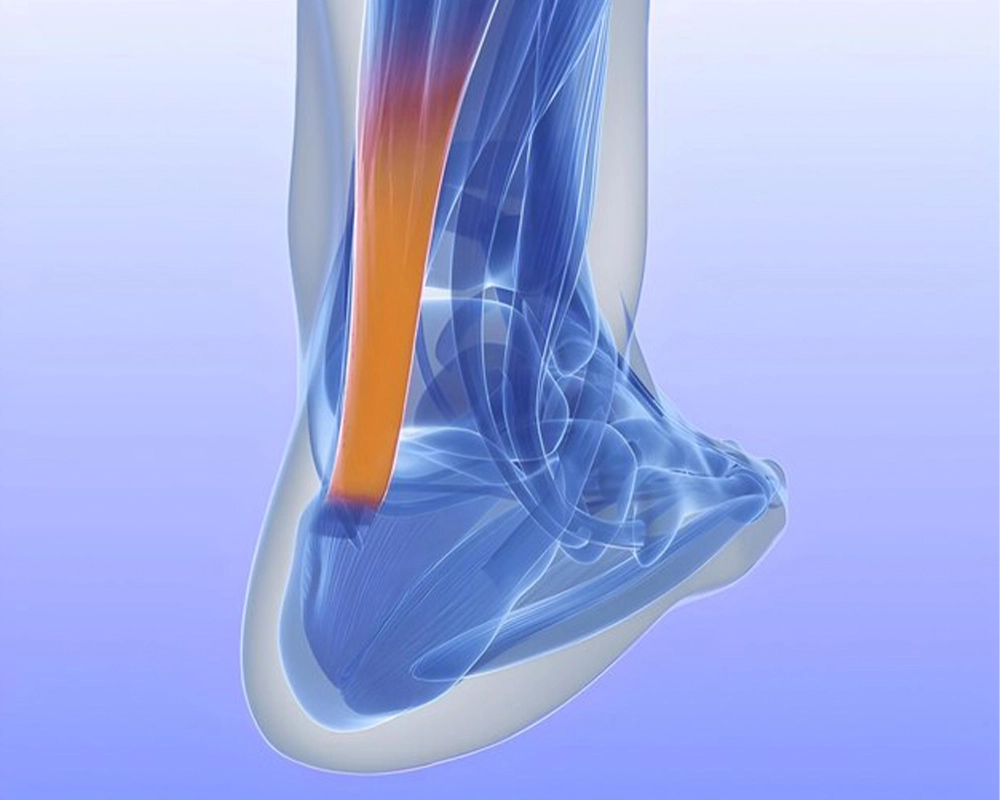
One example of a tendon is your Achilles tendon, which attaches your calf muscle to your heel bone and causes ankle movement. If you have pain and/or swelling in that area, you might have Achilles tendinopathy.
The pain from tendinopathy can interfere with your daily life. For example, it can keep you from playing sports and from doing housework. So, if you have pain or swelling, make sure to contact your healthcare provider for help.
Tendinitis
Tendinitis means inflammation of your tendon. It’s a painful injury that can either be short-term (acute) or long-term (chronic). You may develop tendinitis after a sudden injury from lifting a heavy weight or from repetitive activities that cause micro-tears in your tendon over time.
What are the different tendon conditions?
Tendinopathies are tendon conditions that cause pain and swelling. Some of the most common tendinopathies that healthcare providers see include:
• Achilles tendinitis. Your Achilles is the strongest, largest tendon in your body.
• Patellar tendinitis
• Rotator cuff tendinitis. Other tendinopathies include:
• De Quervain’s tendinosis (tenosynovitis), which affects your wrist and thumb.
• Golfer’s elbow (medial epicondylitis).
• Tennis elbow (lateral epicondylitis).
Who is at risk for tendinopathy?
Tendinopathy affects people of all ages, but some people are more likely than others to develop tendinopathy. Higher risk groups include:
• Athletes.
• People over 40 years old.
• People who do repetitive tasks.
• People who take certain medications.
• People with particular medical conditions.
• People with poor muscle strength.
• Women.
Just having increased risk doesn’t necessarily mean you’ll get tendinitis or tendinosis. Talk to your healthcare provider if you’re concerned.
How common is tendinopathy?
In the general population, tendinopathy affects about 2% to 5% of people. It’s more common in athletes, though. For example, multiple studies have shown that each year around 10% of runners develop Achilles tendinopathy. Furthermore, roughly 50% of all sports injuries are tendon injuries.
What are the symptoms of tendinopathy?
You may have tendinopathy if you’re experiencing pain or tenderness with some or all of the following symptoms:
• Burning.
• Difficulty moving your joint.
• Feeling a crackling or grating sensation when you move your joint.
• Muscle weakness and loss of strength.
• Red, warm skin in the painful area. Please also note that red, warm skin sometimes indicates an infection. If you see this, please contact your healthcare provider.
• Stiffness
• Swelling
What causes tendinopathy?
The exact cause of tendinopathy isn’t always clear. It’s often related to multiple factors. In addition to being in a higher risk group, other risk factors include:
• High-intensity training.
• Muscle imbalances.
• Incorrect training equipment or poor training surfaces.
• Lack of flexibility.
• Lack of strength.
• Too much weight on your tendon (from lifting something).
Tendinopathy can turn chronic if minor injuries occur regularly and don’t heal completely. Repeated activities may cause collagen fibers to break down over time, leading to tendinosis.
Examples of repetitive tasks that can cause tendinosis include:
• Gardening.
• Lifting.
• Landscaping.
• Painting.
• Scrubbing.
• Shoveling.
• Sports.
• Typing.
• Woodworking.
Some medical conditions put you at a higher risk for tendinopathy including:
Dyslipidemia. Dyslipidemia is when your total cholesterol or triglycerides or both are too high.
• Gout.
• Obesity.
• Rheumatoid arthritis.
• Type 2 diabetes.
Common sports associated with tendinopathy include:
• Baseball.
• Basketball.
• Golf.
• Skiing.
• Soccer.
• Swimming.
• Tennis.
How is tendinopathy diagnosed?
Your healthcare provider should go through two steps when you see them about your symptoms: they’ll discuss your history and perform a physical examination. When you talk about your history, your healthcare provider should address:
• The location of your pain.
• The severity of your pain. They’ll ask you to rate your pain on a scale.
• The type of pain (burning, dull, sharp).
• How long you’ve had the symptoms.
During the physical exam, your healthcare provider might:
• Look for redness.
• Look for swelling.
• Test your range of motion (how far you can stretch or move part of your body).
• Touch certain areas to see if you feel tenderness.
Your healthcare provider might diagnose you with tendinopathy based on reported symptoms and the physical exam or, if they need more information, they might order an imaging test such as:
• Ultrasound. An ultrasound reveals changes in your tendon such as thickness, length, stiffness, disorganized and misaligned tendon fibers and tears.
• MRI. Magnetic resonance imaging (MRI) shows the general health or injuries in your tendon.
Quick Contact
Address
1st floor, 2/104, Old Mahabalipuram Rd, Karapakkam, Chennai, Tamil Nadu 600097
lysander.clinic@gmail.com
Mobile
+91 9363396124




